The once-popular mitochondrial free radical theory of aging proved to be too glib. Aging isn’t fundamentally about dispersed damage; rather, dispersed damage is a result when the body’s defenses stand down in old age. Nevertheless, the mitochondria do play a role in aging, largely through signaling and apoptosis. Antioxidants targeted to mitochondria may be an exception to the rule that antioxidants don’t prolong lifespan. And other supplements and strategies that either promote production of new mitochondria or enhance their efficiency of operation show promise for modest lifespan extension.
Growing new mitochondria
A ketogenic diet leads to generation of new mitochondria, as do caloric restriction and exercise. Exercise when the body is starved for sugar (low glycogen) is the most potent stimulator of new mitochondrial growth. Exercise while fasting, or continue to exercise after you “hit your wall”.
Hormones that promote mitochondrial proliferation include thyroxin, estrogens, and glucocorticoids. Promoting new mitochondria has a tendency simultaneously to suppress apoptosis, programmed cell death [ref]. At later ages, apoptosis of cells that are still functional tends to be a larger problem than the failure of cancerous cells to eliminate themselves by apoptosis. In other words, suppressing apoptosis is (on balance) a good thing for anti-aging, but the downside is it can also increase risk of cancer.
Ubiquinone=CoQ10
Coenzyme Q-10 (aka ubiquinone) is an essential part of mitochondrial chemistry, shuttling electrons along their way to the ATP molecules that mitochondria generate as their primary energy export to the cell. It’s often called an antioxidant, but that’s not the primary role of CoQ10.
As a supplement, it is well-established with a good reputation. There is lots of evidence for benefits to health markers, especially athletic endurance, several aspects of heart health, and erectile dysfunction. If you have fibromyalgia or if you are taking statins, CoQ10 is strongly indicated. For chronic fatigue syndrome, it’s definitely worth trying.
But there’s no reason to expect it will increase your life expectancy. Supplementing with ubiquinone increases the lifespan of worms but not mice or rats [ref, ref].
Worms that cannot make unbiquinone live 10 times as long. Just saying…
A few years ago, ubiquinol was introduced as a more bioavailable form of ubiquinone. It’s more expensive, but there is not clear evidence that it is more bioavailable.
PQQ
Pyrroloquinoline quinone is helpful but not necessary part of mitochondrial chemistry. Bacteria make a lot of it; plants less; mammals only tiny quantities. Mice completely deprived of PQQ show growth deficiency, but the amount that they need is tiny compared to the quantities in PQQ supplements.
PQQ is a growth factor for bacteria, and the principal health claim for PQQ is that it can stimulate growth of new mitochondria. The evidence is based on biochemistry and cell cultures. In live mice, it has been shown that PQQ deficiency results in a mitochondria deficiency, but not that large quantities of PQQ lead to more mitochondria.
Bill Faloon (LEF) and Joseph Cohen (selfhacked) are big fans of PQQ, and you can read a list of benefits here. Cohen claims PQQ helps with sleep quality and nerve growth, leading to better cognitive function.
Small quantities of PQQ can be absorbed from many plant foods, but not animal foods. Much larger quantities come in supplement form. 100 g of tofu has just 2µg (micrograms). Supplements are usually 5-20 mg, hundreds of times as much as you’re likely to get from a vegetarian diet. Here is a table of PQQ concentrations in foods:
SkQ and MitoQ
These are two closely related molecules, originally synthesized in Russia in the 1970s, but it wasn’t until the 1990s that their therapeutic value was documented by two New Zealand scientists. One end of the molecule is CoQ10 (or a version found in plants, claimed to be even more powerful as an antioxidant). The other end of the molecule is an electric tugboat that pulls the molecule into mitochondria.
I’ve written a detailed report three years ago. At the time, I noted that the Russians claimed to extend lifespan of mice modestly with SkQ, and SkQ was found (also in Russian labs) to be a powerful rejuvenant for aging eyes. The Russians sell SkQ as eye drops. The Kiwis sell MitoQ as skin cream and also as pills.
Earlier this year, the Russian labs announced that SkQ had substantially extended lifespan of a mouse strain that was short-lived because of a mitochondrial defect. None of the Russian claims have been reproduced in Western labs. Three years ago, I was inclined to give the Russians the benefit of the doubt, but now I’m starting to wonder, since the New Zealand company has a laboratory arm, and they haven’t announced anything nearly so impressive.
Humanin and her sisters
Mitochondria have ringlets of their own DNA, encoding just 37 genes. (That doesn’t mean that the mitochondria only need 37 proteins; the great majority of proteins needed by mitochondria are coded in chromosomes of the cell nucleus, and transported to the mitochondria as needed.) Just 16 years ago, the first mitochondrial-coded protein to be discovered was named Humanin, because it was found to improve cognitive function to dementia patients, restoring some of their “humanity”. In addition to being neuroprotective, humanin promotes insulin sensitivity. Humannin’s action is not confined to the mitochondrion in which it was produced, but in fact it circulates in the blood as a signal molecule. Blood levels of humanin decline with age.
Humanin
In experiments with mice, humanin injections have been shown to protect against disease. Lifespan assays with humanin are not yet available.
To date, HN and its analogs have been demonstrated to play a role in multiple diseases including type 2 diabetes (25, 43), cardiovascular disease (CVD) (2, 3, 47), memory loss (48), amyotrophic lateral sclerosis (ALS) (49), stroke (50), and inflammation (22, 51). The mechanisms that are common to many of these age-related diseases are oxidative stress (52) and mitochondrial dysfunction (53). Mitochondria are major source of ROS, excess of which can cause oxidative damage of cellular lipids, proteins, and DNA. The accumulation of oxidative damage will result in decline of mitochondrial function, which in turn leads to enhanced ROS production (53). This vicious cycle can play a role in cellular damage, apoptosis, and cellular senescence – contributing to aging and age-related diseases. Indeed, oxidative stress is tightly linked to multiple human diseases such as Parkinson’s disease (PD) (54), AD (55), atherosclerosis (56), heart failure (57), myocardial infarction (58), chronic inflammation (59), kidney disease (60), stroke (61), cancers (62, 63), and many types of metabolic disorders (64, 65). We and others have shown that HN plays critical roles in reducing oxidative stress (66–68). [2014 review]
Pinchas Cohen, MD (Dean, School of Gerontology, University of Southern California Davis, Los Angeles, California) is an expert in humanin, a protein (peptide) produced in mitochondria. Mitochondria are energy-generating organelles in cells, which have their own DNA separate from the DNA in the nucleus. The amount of DNA found in the mitochondria is much less than that found in the nucleus. As such, mitochondrial DNA contains codes for only a few proteins, humanin being one of them. Humanin was discovered by a search for factors helping to keep neurons alive in undiseased portions of the brains of Alzheimer’s disease patients. Humanin protects neurons against cell death in Alzheimer’s disease, as well as protecting against toxic chemicals and prions (toxic proteins)[ref]. Dr. Cohen’s team has shown that humanin also protects cells lining blood vessel walls, preventing atherosclerosis. In particular, they have shown that low levels of humanin in the bloodstream are associated with endothelial dysfunction of the coronary arteries (arteries of the heart).[ref] Humanin has also been shown to promote insulin sensitivity, the responsiveness of tissues to insulin. Because humanin levels decline with age, it is believed that reduced humanin contributes to the development of aging-associated diseases, including Alzheimer’s disease and type II diabetes. [Ben Best]
Personal notes: This lab near where I am visiting in Beijing is taking leadership in characterizing a group of short peptides similar in origin to humanin, and this company across the street from us is selling mitochondrial peptides.
If humanin were a patentable drug, there would be much excitement and multiple clinical trials for AD, probably leading to expansion into general anti-aging effects.
MOTS-c
This is another short peptide of mitochondrial origin, only recently discovered and characterized. I was alerted to its existence by a study from a USC lab that was written up here in ScienceBlog just this month (reprinted from a USC press release). Results are new but impressive. Mice injected with MOTS-c had more muscle mass, less fat, more strength and endurance. MOTS-c protected their insulin sensitivity when mice were fed a high fat diet [ref]. Lifespan studies haven’t been done yet.
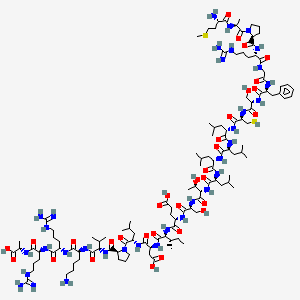
Like humanin, MOTS-c is manufactured inside mitochondria from a template in mitochondrial DNA, but it is exported from the cell and appears in the bloodstream as a signal molecule. Blood levels of MOTS-c decline with age. It is a mini protein molecule with 16 amino acids, too big to survive digestion so it can’t be taken orally.
“MOTS-c holds much potential as a target to treat metabolic syndromes by regulating muscle and fat physiology, and perhaps even extend our healthy lifespan.”[ref]
Let’s keep your eyes on this one over the next year or two.
Gutathione / NAC
I’ve never heard anyone say a bad word about glutathione. It’s the antioxidant with no downside. Genetic modifications that upregulate glutathione have increased lifespan in worms, flies and mice.
For a long while, it has been assumed that you can’t eat glutathione, because it doesn’t survive digestion. Some researchers at Penn State disagree, finding impressive increases in tissue and blood levels when people were supplemented with up to 1 g per day raw glutathione. Liposomal glutathione is an oral delivery form that gets around the digestion problem, especially when taken with methyl donors like SAMe.
The herb Sylimarin=milk thistle may increase glutathione. For now, the precursor molecule N-Acetyl Cysteine (NAC) is the best-established supplement we have to promote glutathione. In the one available study, supplementing with NAC greatly increased lifespan in male but not female mice. NAC also increases lifespan in worms and flies.
-N-Acetylcysteine_Structural_Formulae.png)
N-Acetyl Cysteine

Glutathione
For the future, we might hope to do better. Less than 20% of the cell’s glutathione actually makes its way to the mitochondria, where it is most needed. There are esters of glutathione that, in theory, ought to be attracted into the mitochondria. They have been tested in cell culture only, but are more than ripe for animal testing [ref].
Nicotinamide Riboside (NR) and other NAD+ enhancers
The chemicals NAD+ and NADH are alternative, cycled forms of an intermediate in the process by which mitochondria make energy. Levels of NAD+/NADH decline with age. NR is a precursor to NAD+, and it has been demonstrated (preliminary results in humans) that NR supplementation increases blood levels of NAD+.
It may be awhile before we know for sure whether this leads to better health or longer lifespan. Niagen and Basis are heavily promoted with credible scientifists behind their products, and many early adopters offer subjective reports of short-term benefits. There is one mouse study claiming to pull a 3% extension of lifespan out of the noise, and perhaps I am less open to the finding because the article, published prominently in Science, seems so breathless in describing benefits.
Melatonin
The primary role of melatonin is to regulate the body’s sleep/wake cycle. Melatonin declines with age and the timing of our daily melatonin surge gets fuzzier and less reliable with age.sleep quality deteriorates. Sleep quality suffers.
Melatonin is well-established in mice as a modest longevity aid, although results have been inconsistent. 12 out of 20 studies showed a lifespan increase, and the remaining 8 showed no increase or decrease. Whether nightly supplementation affects mortality rates in humans has never been determined.
Melatonin is concentrated in mitochondria as much as 100-fold, and it may even be created there [ref], independent of the circulating melatonin that is secreted from the pineal gland at night. One of its actions is as a mitochondrial antioxidant and scavenger of ROS.
Twenty years ago, Walter Pierpaoli promoted melatonin as a sleep aid, cancer fighting hormone that would enhance your mood and your sex life while keeping you young. Russian labs have also been optimistic. My take is that melatonin is a legitimate anti-aging hormone, and is especially useful for those of us whose sleep is disrupted with age. It is widely available, cheap and safe. Unless you’re fighting jet lag, 1 to 2 mg at night is all you need.
Also worth mentioning
Magnesium is required for manufacture of glutathione. Selenium works along with glutathione. Omega-3 fatty acids can promote synthesis of glutathione. Acetyl L-carnitine transports fat fuels through the mitochondrial membrane. Alpha-lipoic acid is part of the mitochondrial energy metabolism.
The Bottom Line
Commercial interests can make some messages louder than others, and the health news we hear is affected by what is profitable as much as by what is healthy. Exercise is primary, but has no sales value. Of the supplements reviewed here, NAC is the best-established for mitochondrial health and a possible effect on lifespan. It is cheap and available. Liposomal glutathione is certainly more expensive and possibly more effective. Melatonin is even cheaper, and has been found to increase lifespan in multiple rodent studies, with broad benefits apart from modification of mitochondrial function. Humanin and MOTS-c, not yet close to commercial availability, seem to be promising substances to explore for health, though not for profits.



